COVID control chiefs set to tighten mask rules for hotel quarantine staff
Controversial national rules that mean healthcare and quarantine hotel workers are allowed to wear a simple surgical mask when treating COVID-positive patients are set to be overturned.
Some of the hotel quarantine workers who have been infected with COVID-19 in Australia this year were wearing only a surgical mask, or even no mask, and the regulations have been heavily criticised by the Australian Medical Association.
The move to tighten the rules has been under consideration by Australia’s Infection Control Expert Group for two weeks, after being approved by all 32 member organisations of the National COVID-19 Clinical Evidence Taskforce.
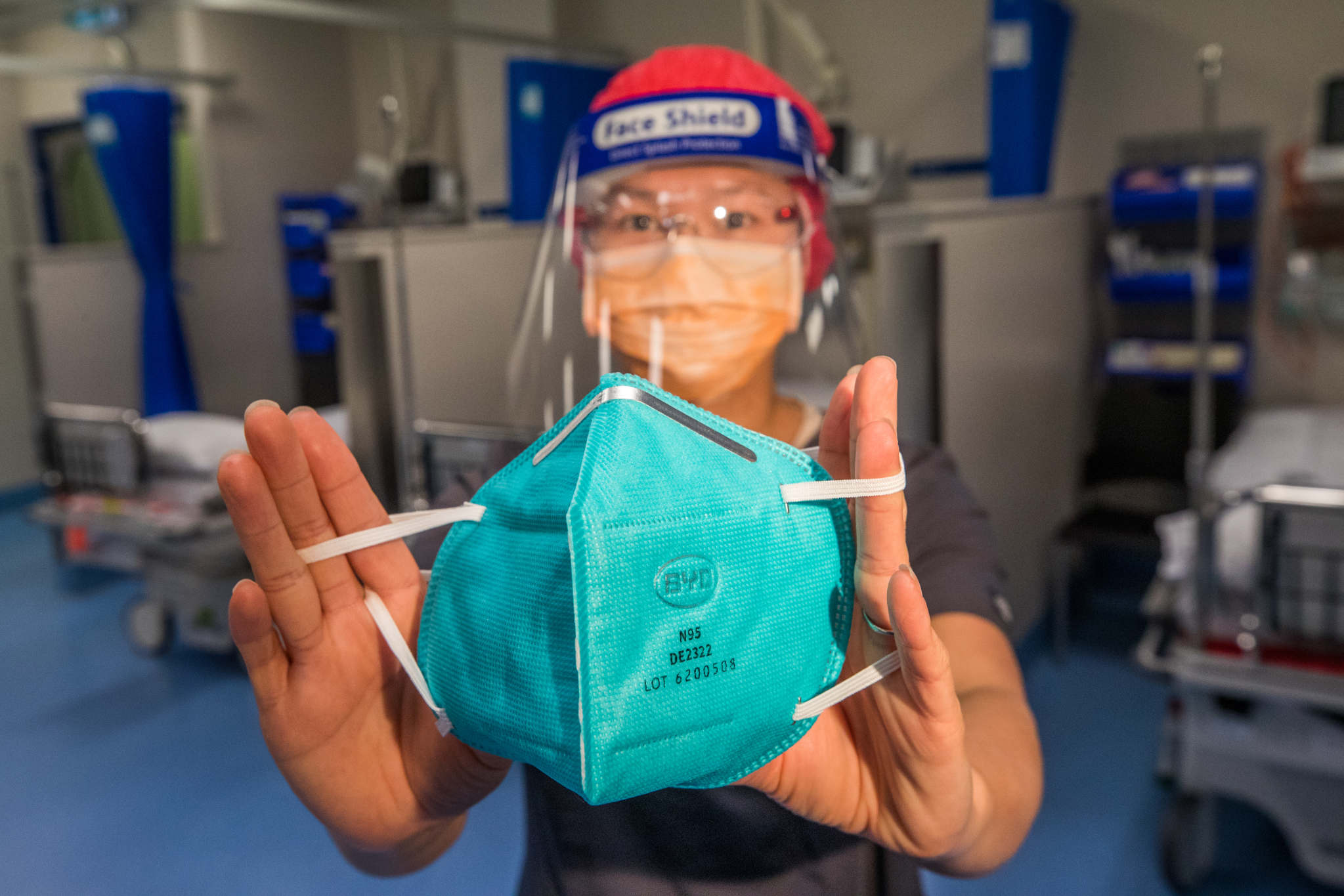
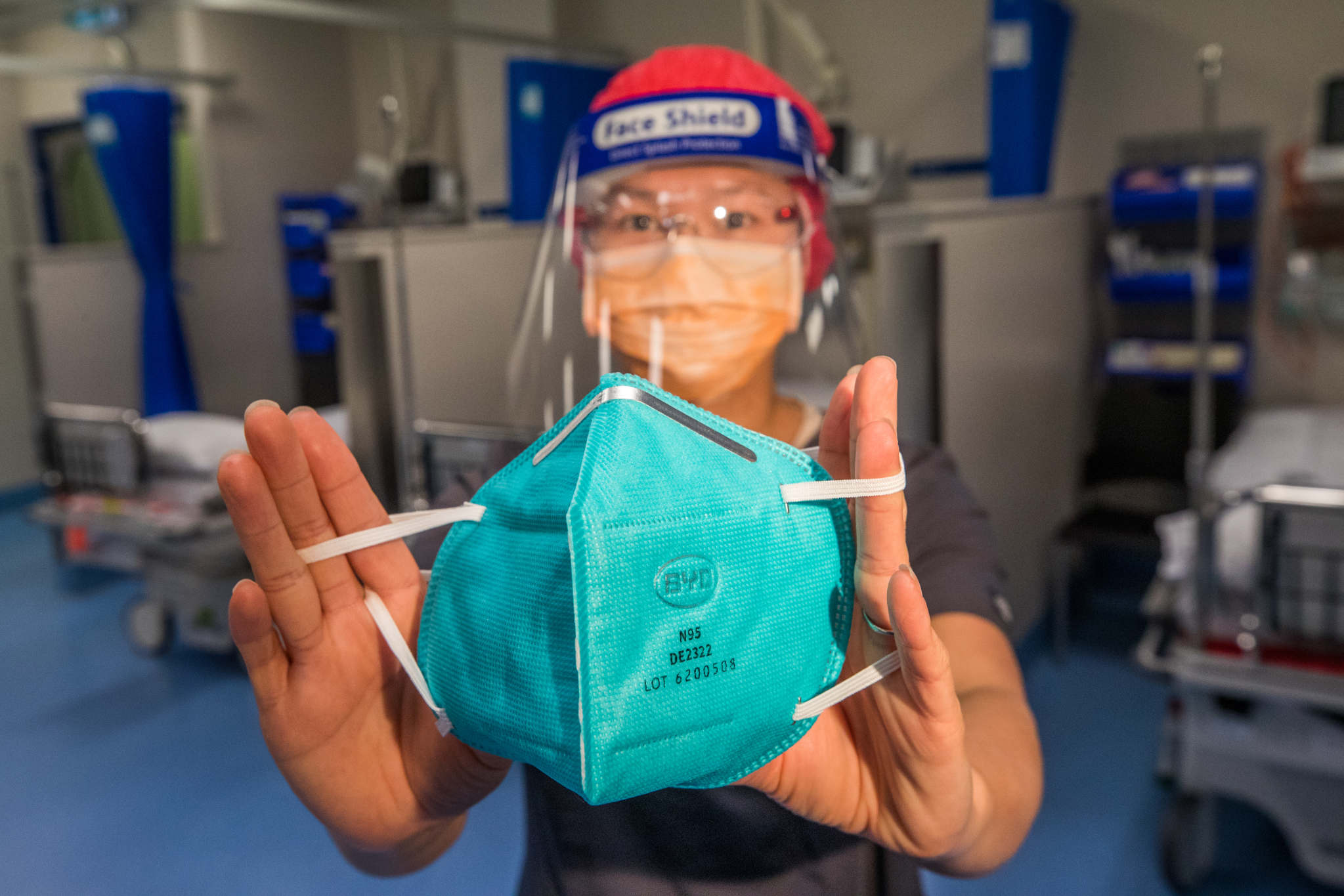
AMA president Omar Khorshid expects the change, to be announced in the next few weeks, will recommend or require that N95 masks, goggles, gowns and gloves be used in interactions with patients with COVID-19, or those suspected to have it.
“If we don’t see it, we would be very upset,” he said. “There were a lot of weasel words in the previous recommendations that basically meant for routine care, people were wearing surgical masks, [and] we’ve seen transmission in those settings.”
Many states now provide N95 masks to hotel quarantine workers, though as recently as this month this was not the case for security guards working in Perth facilities, despite warnings that surgical masks do not provide adequate protection against coronavirus for high-risk workers.
“While we can’t prove that an N95 mask will stop transmission, we are expecting the new guidelines will make it clear that that is the expectation,” Dr Khorshid said.
Current advice from the Infection Control Expert Group, last updated in March, allows surgical masks with protective eyewear to be used at a minimum in the routine care of patients with suspected or confirmed COVID-19, including in hotel quarantine.
It says N95 masks or equivalent should be used only when indicated by a risk assessment, while they are specifically recommended for some workers, including those performing aerosol-generating procedures (such as an intubation or tracheotomy) on suspected or confirmed COVID patients.
The advice continues to be a point of contention in a heated public debate between leading infectious diseases figures in Australia about the relative risk of airborne transmission of coronavirus.
In a speech this week, Australia’s former deputy chief medical officer Nick Coatsworth argued it was a myth that government advice had ignored the risk of aerosol transmission of COVID-19.
“It is a phoney war because the real issue is about tolerance of risk,” he said.
It’s estimated that almost 3000 people were infected with COVID-19 while working at health facilities in Victoria last year, as N95 masks were reserved for those considered at highest risk of infection.
Health workers campaigned for masks to be tested to ensure they properly protected each wearer, a practice that often did not occur despite being required by Australian standards.
The federal Health Department confirmed the Infection Control Expert Group was considering the consensus recommendations on face masks and eye protection from the taskforce.
“As with all documents that ICEG is asked to review, these recommendations will be given thorough and appropriate consideration before a response is provided to the COVID Clinical Evidence Taskforce,” the spokesman said.
Australian Institute of Occupational Hygienists president-elect Kate Cole, who sits on the taskforce’s panel on infection prevention and control, said if the recommendations were adopted there should be a reduction in outbreaks from quarantine.
“The real impact is that we can expect to stop seeing outbreaks in hotel quarantine of workers who then unintentionally bring that virus into our community,” she said.
Source: The Sydney Morning Herald




